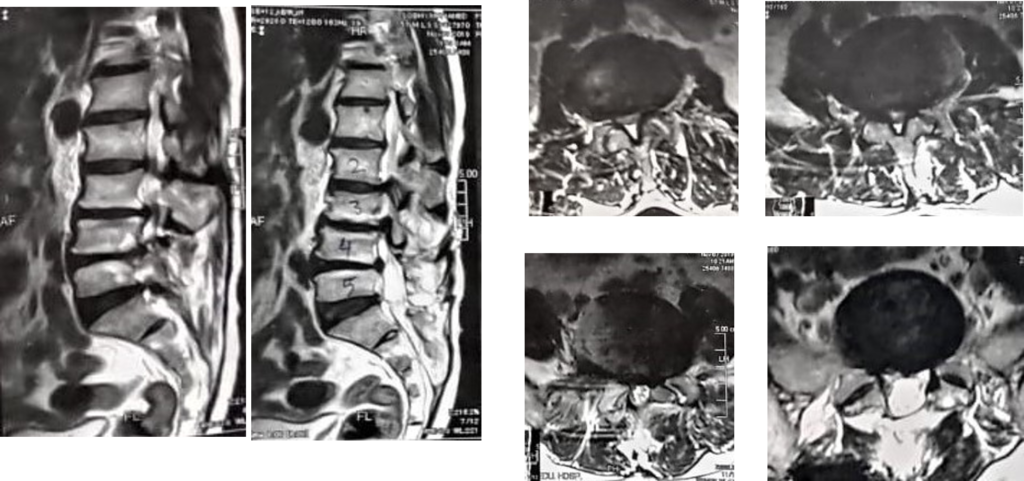
•57 years old male with severe low back pain. He has history of L4-5 discectomy 27 years ago. Otherwise neurologically intact.
•What do you recommend in such a case?
Thank you for putting this together …
I would analyze clinically the type of this severe local back pain to get to know the source of pain whether:
1- I’m dealing with discitis type of pain and prove it further with ESR / CRP and T1 + gadolinium studies
Then management can be IV antibiotics 6-8 weeks based on blood culture followed by oral for another 6 weeks before considering intervention
OR
2- I’m dealing with intractable degenerative scoliosis that requires a big deformity surgery (T10 – L5) with 1 or 2 TLIF at L3/4 & L4/5 (after failure of 6 months of conservative management including steroid local facet injections, physiotherapy, opioid analgesia … etc ). Multilevel decompression laminectomies and bilateral facetectomies at L2/3/4 will facilitate mobilizing the spine intraop and TLIF cage insertion at the required levels ideally the lower levels to gain some lordosis matching the patient’s pelvic incidence measurement.
If radicular symptoms were more dominant, microdecompression of stenotic levels via hemilaminotomies at 2 or 3 levels could be enough to avoid long segment instrumentation and fusion that may lead to PJK …..
Sincerely, A. Bayoumi
Thanks Ahmed
He has no radicular symptoms
I think he need to be corrected from T10 -iliac screws with L3-4 L4-5 TLIF and L5-S1 PLIF
What’s your opinion Prof Zileli
You’re welcome
If you wanna extend down to sacropelvic fixation because of the L5/S1 black disc, you can consider the S2AI screws instead of iliac screws . It doesn’t require additional rods , lateral muscle dissection or offset connector .
Entry point between S1&S2 lateral margin of dorsal foramina and going caudal and laterally above the greater sciatic notch aiming to AIIS or just above
Diameter 8-10 mm, length 80 to 100 mm
It comes in line with S1 Pedicle Screw entry point , but trajectory is more laterally horizontal about 40 degrees
Kind regards,
A. Bayoumi
Very nice discussion. I respect all ideas. I have following comments:
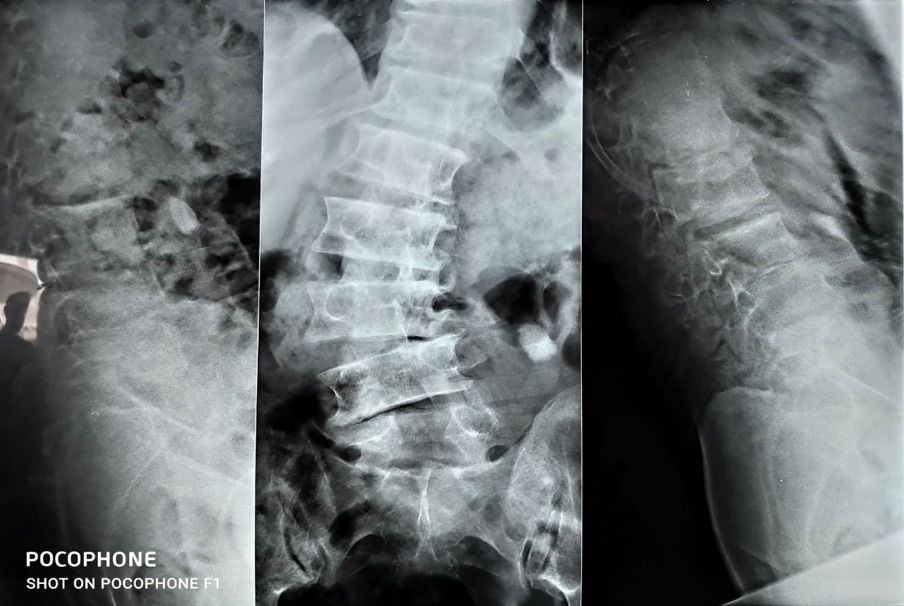
1-In any deformity case, we must have whole spine AP and lateral radiograms to see and measure the sagittal and coronal balance.
2-Besides, the presenter should note if the patient has anteflexion posture or scoliosis in erect position.
3-This patient has no radicular symptoms, just have axial back pain. Lumbar injections (facet injection, sakroiliac injection) may have transient benefits.
4-A deformity surgery will be more beneficial. Age of the patient and being a male (possibly no osteoporosis) are some good points. I also admit to perform a long fixation from T10 to S1. Since he had a previous laminectomy at L5 and disc height is preserved, L5-S1 motion segment should better be added to the construct. Iliac screws are necessary then. 3 levels interbody fusion with cages would prevent a nonunion at the lower level. In any case, a PJK may happen, and the patient must be informed about this complication as well.
I would like to hear Onur Yaman’s comments on this case.
Sincerely
Mehmet Zileli
Dear Zileli and Collegues,
First, we have to decide the type of the surgery. Will it be a decompression or will it a deformity surgery ? I think it will be a deformity surgery. For a spinal deformity case we need more details. As Zileli has mentioned we need standing AP and lateral scoliosis X rays to see the relationship of the head and pelvis. We also need lateral bending x ray.
1. Does the patient have sagittal imbalance?
2. Does the patient have coronal imbalance ? If yes? Is it coronal or convex coronal imbalance?
These questions have to be answered before planning the surgery. Because everything will be changed.
But according only to these data, X rays says that:
1. Patient is using retroversion to maintain sagittal balance. Because the endplate of sacrum is nearly parallel to floor. (Patient is trying to keep the head over pelvis) We can not see the femoral heads. So how can we decide the degree of the lordosis that is suitable for this patient. If we see the femoral heads on X-ray we can measure the pelvic incidence and we can decide it the proper lumbar lordosis with PI +/- 10 degrees. Pelvic incidence is like the finger print. It changes from patient to patient. (Every custom can not wear the same size jacket)
2. On the AP view we can not decide the coronal imbalance so we can only guess it. Patient may have concave coronal imbalance. (If the plumb line drawing from C7 or T1 falls to the concave side of the lumbar curve) And there is a fractional curve which apex is L5. Without correcting that fractional curve patient will fail after the surgery. Dr.Onur Yaman continous
Knowing the coronal imbalance will change your surgical strategy.
If it is concave coronal imbalance correcting the main curve will correct the coronal imbalance if it is convex coronal imbalance correcting directly lumbar main curve will worsen postoperative coronal imbalance.
Other point are the flexibility of the main curve, the flexibility of the lumbosacral junction and degeneration of the L5-S1 disc.
There are lots of details we don’t know. But T10- iliac will be a possible solution. L4 on the coronal view has to be parallel to floor. Fractional and also lumbar curve has to be corrected. I don’t know the correct answer because I can see only the leg of the elephant as the story ‘Elephant in the Dark’ from Jalal al-Din. I have attached this picture below.
Kindest regards. Onur Yaman